 November 25, the Science and Engineering Fellowship heard from Dr. Jeff Wilusz of the Department of Microbiology, Immunology and Pathology at Colorado State University. Twenty-seven members listened as Dr. Wilusz summarized the technology, including both tried-and-true and ground-breaking approaches, that are being used in the search for a vaccine for Covid-19.
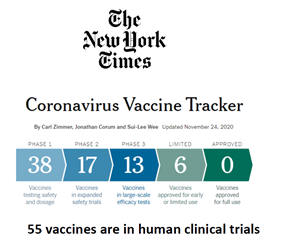
November 25, the Science and Engineering Fellowship heard from Dr. Jeff Wilusz of the Department of Microbiology, Immunology and Pathology at Colorado State University. Twenty-seven members listened as Dr. Wilusz summarized the technology, including both tried-and-true and ground-breaking approaches, that are being used in the search for a vaccine for Covid-19.Dr. Wilusz introduced his talk by indicating there are currently 55 vaccines for Covid-19 in the works, and up to 150 candidates being developed. He said the first vaccine out of the box is from China and consists of a chemically inactivated virus grown in tissue culture, then killed, purified and used as a vaccine (the conventional approach used for many years).
A few early vaccines instead use an adenovirus (a common virus) approach, wherein a part of the adenovirus DNA has been replaced with the Covid-19 spike protein and used as a vaccine. This approach was used in a failed genetic engineering experiment in which the patient died from vaccine complications, so is unlikely to be approved.
The Russians have a vaccine called Sputnik V, using a two phase adenovirus approach. The first phase uses an Adenovirus 26 strain and a Covid-19 insert. The second phase uses a different Adenovirus (strain 5) also with a Covid-19 insert. Sputnik V appeared to be released without clinical trials by an authoritarian government.
The AstraZeneca vaccine uses a simian (monkey) adenovirus strain expressing a full-length Covid-19 spike protein. Using a simian adenovirus has advantages over human adenovirus strains because it is quite stable and relatively inexpensive. It was developed rapidly because the Astra scientists were already well along developing a vaccine against MERS, a related coronavirus of a few years ago.
An unusual approach is the use of the tuberculosis BCG vaccine since it appears persons having received the BCG vaccine have a lower susceptibility to Covid-19. This approach is interesting but is not likely to gain traction.
Dr. Wilusz indicated there are 5 vaccines being developed using mRNA technology. Most of them use a similar approach. Basically, modern genetic sequencing technology is used to create an RNA molecule (with variations depending on the company), the mRNA is encapsulated into a lipid droplet used to deliver the mRNA to a cell, after injection, the droplet is taken into the host’s cell, a messenger RNA then is directed to make the Covid-19 spike protein which is then the basis for developing antibodies in the host. Early trials using the Pfizer mRNA vaccine shows the body makes a large amount of antibody that persist for weeks if not months.
Somewhat as an aside, Dr. Wilusz discussed the difference between using a DNA based vaccine and an RNA based vaccine. The RNA approach does not involve the host cell’s nucleus, minimizing genetic damage or changes. Similarly, there’s no concern for insertional mutagenesis, in which new bases are inadvertently introduced to the incoming DNA leading to unwanted mutations. The mRNA is translated and expressed immediately. The mRNA is a short-term treatment, meaning the effect is transient and does not lead to long-term changes in the cell. Drawbacks to the mRNA approach involve the relatively long-understood problem that foreign mRNA leads to aggressive immunostimulation – meaning the body reacts to the new genetic material in a harmful way. The breakthrough, which in my opinion may be Nobel-prize stuff, is the realization that the incoming mNA must be modified in a process called methylation – bases have to have tiny chemical changes that cause the host cell to think the new RNA is not “foreign” and rapidly destroyed. All of the new mRNA vaccines take this methyation into account in one way or another.
Dr. Wilusz finished on a related note, talking about the possibility cancer therapy may use this mRNA approach to start personalized treatment of melanoma. The problem is that melanoma mutates – a melanoma may be successfully treated, but a variant pops up and everything starts all over to the detriment of the cancer patient. The new treatment being developed involves extracting mRNA from an individual’s melanoma cells, putting up to 5 mRNAs from that melanoma into a vaccine mRNA (a polyvalent vaccine, so to speak), then immunizing the patient against the 5 possible mutations that might come from the original tumor. This approach is quite individualized and personalized, in that my melanoma will be quite different from my neighbor’s, hence it will only work with my tumor and not his. This is an exciting possibility, but will require lots of work, not to mention headaches for the FDA to approve such an individualized approach.
Dr. Wlusz was asked which vaccine he would take, if offered. He was firm in supporting one of the mRNA vaccines over an adenovirus-ba